A Case of Necrotizing Pancreatitis
Dr. Tanjila Nawshin, Dr. Mir Atiqur Rahaman, Sajal, Dr. Md. Maniruzzaman
This case is about a 59 year old hypertensive gentleman. According to the attendant’s statement, he was reasonably well till 08.11.2013 when he developed severe abdominal pain with two episodes of vomiting.
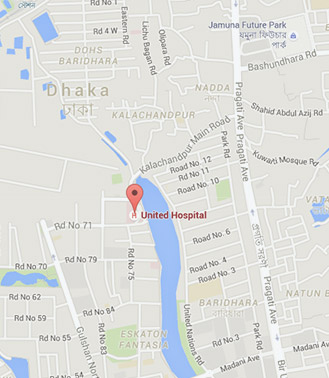
He was then taken to a local hospital. On 10.11.2013, he developed shortness of breath and his conscious level deteriorated. He was then intubated and kept on mechanical ventilator. CT scan of whole abdomen revealed acute necrotizing pancreatitis with diffuse collection in different spaces in the abdomen. On 19.11.2013, the patient was taken to United Hospital for further management and admitted into the GICU.
On admission in GICU, he looked toxic – Pulse: 85/min; BP: 105 / 79 mm of Hg, Temp: 101*F, R-R: 20 br / min, SpO2: 94 % with FiO2 50%. His abdomen was distended, tense and the bowel sound was absent. Auscultation of lungs revealed basal crepitations.
Patient underwent laparotomy followed by pancreatic necrosectomy, fixation of closed cavity lavage system in lesser sac and cholecystectomy. Left paracolic, pelvic and right sub-hepatic drains were fixed. Irrigation of the closed cavity with peritoneal dialysis fluid started from 22.11.2013.
Weaning trial was done several times but failed as the patient developed hypoxaemia. Patient was continuously febrile. On 28.11.2013, he was extubated and kept on Bi-PAP intermittently for positive pressure support. He received breathing exercise and limb physiotherapy regularly as well as TPN.
In GICU, he developed fever and his WBC count was high. Tracheal Aspirate C/S showed growth of Acinetobacter. He received injections Carbapenam, Piperacillin, Colistin, Vancomycin and Netilmycin to counteract this new growth.
On 08.12.2013, he developed high fever, hypotension, hypoxaemia and became drowsy. Patient was re-intubated electively and kept on SIMV-PC. His urine output became low, USG of W/A showed renal parenchymal disease. Renal function deteriorated with metabolic acidosis and SLED was given. Patient’s LFT became abnormal and he got mildly disoriented. His S. Procalcitonin was 24.6 which indicated septic shock. Urine and peritoneal dialysis fluid C/S showed growth of Candida. He was given peritoneal flush with Amphotericin B and injection Xeroder I/V.
Abdominal clips and the sub-hepatic drain tube were removed. Feeding trial was given and tolerated. From 12.12.2013 he was haemo-dynamically stable. T-piece is an oxygen delivery device for tracheostomy patients. The patient was given T-piece trial which was satisfactory and accordingly the patient was extubated on 18.12.2013. He was conscious, mildly disoriented, haemo-dynamically stable, afebrile and was able to maintain SpO2 in room air. He was then shifted from GICU to GHDU on 31.12.2013 as his condition was no longer life threatening.