A young female presented with shortness of breath
Dr. Shafiqul A&E
A 20-years female normotensive nondiabetic healing from comilla presented in A&E department with SOB for 1 month, severe for 1 day. She was alright 2 years back, then she developed localized swelling and itching which was gradually involve her whole body, for that she was repeatedly consult with physician and was treated with antihistamin and some other drugs which was white in colour but the name could not mention though her symptom did not resolve completely.
But for the last 1 month she developed SOB, multiple joints pain, low grade intermittent fever, rash over whole body, oral ulcer and sudden developed hearing loss for 3 days. SOB was initially mild then gradually become severe for 1 day. SOB was associated with dry cough and sometimes with productive mucoid sputum . Joints pain involved small and large joints of both upper and lower limbs, which was inflammatory in nature. Rash involved whole body including face, which was increase after exposure to sunlight. She had oral ulcer mostly in the hard palate for one and half month.
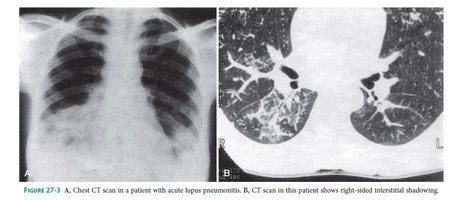
There was no h/o convulsion, unconsciousness, Reynaud's, blood transfusion, family h/o of such type of illness , contact with known TB pt. O/E: Pt was ill looking, severely dyspnic, was non communicative, Cyanotic , Anemic, Malar rash, Alopecia , Multiple hyperpigmented lesion over whole body, Oral ulcer in hard palate, Leg edema +, Pulse-120bpm, Bp -100/60 mm of hg, RR- 35 breath/min, Temp -99°F, Pso?-78%, Bed side urine test – was not done, Respiratory system-bil basal crackles, MSK- grade-3 tenderness small and large joints of both upper and lower limbs, Ophthalmoscope exam and Hearing test was not done, Other systemic exam- normal .Clinical dx- SLE with Acute lupus pneumonitis/pulmonary embolism/Acute alveolar haemorrhage/cryptogenic organiging pneumonia with respiratory failure ,?lupus nephritis, MSK, Mucocutenious, Ear involvement.
Investigation done from outside CBC –Hb-8gm/l, ESR-110 , S. creatinin-1.6mg/dl, CxR –bil lower zone hazyness with bit minimal plural effusion with minimal pericardial effusion, Urine RME, UTP, ANA, Anti ds DNA, CRP, C3, C4, Sputum for gm staining, c/s, Blood c/s ,BAL, HRCT chest – was not done as because pt was transfered to govt hospital for financial constraint.
- Lupus emergencies are RPGN, Acute myelopathy, Severe acute confusional state, Pneumonitis with resp. failure, Alveolar hemorrhage, Optic neuritis and severe lupus includes Class IV LN, Encephalitis, psychosis, coma, myelopathy, Platelet <15,000,Severe pneumonitis, pulmonary hemorrhage, Cardiac tamponade, severe myocarditis.
- Management: Hospitalization, Methylprednisolne 1 gm iv daily for three consecutive days, followed by oral prednisolone 0.5-1 mg/kg/d Continued till activity remains completely suppressed, Usual duration: 6 to 10 weeks , IV pulse cyclophosphamide 500 mg/m2 IV 4-wkly for (3 to) 6 months or mycofenolate2-3 gm/d for induction, switch over to less toxic SSAs, eg., AZT or MMF . Stopped after 2-year flare-free interval, Left on an antimalarial.