Case Report: Post Dengue Guillain Barre Syndrome (GBS)
Dr Afsana Begum, Dr Safia Binte Rabbani
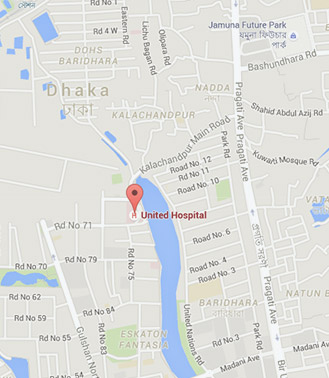
Dengue, an acute viral disease transmitted by Aedes mosquitoes, is highly endemic in many tropical and subtropical areas of the world. Various types of neurological manifestations are described in dengue fever, of which peripheral neuropathy or GBS is rarely reported. This is the second case of post-dengue GBS reported from United Hospital in Bangladesh.
A 56-year-old South Korean man presented with fever, body ache, headache and skin rash for 2 days. There was no history suggestive of mucocutaneous bleeding. On clinical examination, patient was dehydrated; having generalized maculopapular rash more marked in face and trunk, his temperature was 99.4ºF. Investigations showed hemoglobin of 15.2 g/dl, total leukocytes count 2300/mm and platelet count 1,20,000/mm. Dengue NS1 was positive. He was conservatively managed and discharged from hospital. Four days later, the patient developed weakness and numbness of all four limbs associated with areflexia in lower limb. Muscle power was grade 2/5 in lower limbs and grade 3/5 in upper limb. There was no clinical involvement of cranial nerves, sensory system, or autonomic nervous system initially. His serum potassium level was 3.15 mmol/L which was corrected by potassium supplementation. Nerve conduction study showed mixed motor and sensory peripheral neuropathy consistent with GBS. Cerebrospinal fluid analysis showed 3 leukocytes/mm, protein 194.57 mg/dl, and sugar 5.02mmol/L. A diagnosis of GBS - acute motor-sensory axonal neuropathy (AMSAN) variant - was made and a 5 days course of intravenous immunoglobulin was given. During this time patient was also put on mechanical ventilation due to development of respiratory failure as well as supraventricular tachycardia along with hypertensive heart failure. Later the patient was shifted to South Korea under support of artificial ventilation by air ambulance as per the wish of his guardians.
Neurological complications in Dengue are hypothesized to occur through three pathogenic mechanisms:
1) Neurotropism leading to encephalitis, meningitis, myositis and myelitis, 2) Systemic complications resulting in encephalopathy, stroke and hypokalemic paralysis and 3) Postinfectious immune-mediated ADEM, GBS and optic neuritis.
GBS is a post-infectious polyradiculopathy known to occur in post-gastrointestinal infection with Campylobacter jejuni and other infective agents, like Mycoplasma, CMV, EBV and Herpes virus. It rarely occurs due to demyelination in post-dengue infection. So, in conclusion, patients presenting with GBS in whom no usual antecedent infections are identified, screening for dengue virus infection may help in identifying a rare cause.