Pigmented Villonodular Synovitis - a rare benign joint disease, a diagnostic challenge
Dr Shakila Parveen
A 40yrs old male patient with history of right knee pain, swelling and restricted movement for about a week presented at orthopedic department of United Hospital. He had history of trauma 15 years back at the same knee joint. On physical exam he had restricted movement, joint effusion, palpable mass and gross swelling of right knee joint but no muscle weakness.
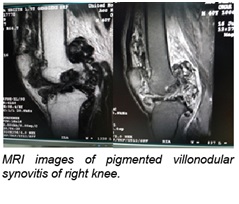
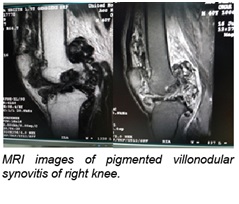 Subsequently MRI and X-ray of right knee joint was done at Radiology Department. On MRI, right knee joint was found swollen, numerous irregular heterogeneous and mixed signal intensity areas were noted within and outside synovial cavity forming a mass lesion with ill defined margin extending above up to the anterior aspect of lower thigh. Focal hyper intense areas were seen in the condyles of tibia and femur on PDFS and STIR images suggesting bone oedema. Bony irregularities were also noted in the tibial and femoral condyles with joint space narrowing. All menisci and ligaments of the knee joint were of normal configuration and signal intensity. All these findings suggested this to be a case pigmented villonodular synovitis (PVNS) of right knee joint. X ray showed osteoarthritic changes of knee joint.
Subsequently MRI and X-ray of right knee joint was done at Radiology Department. On MRI, right knee joint was found swollen, numerous irregular heterogeneous and mixed signal intensity areas were noted within and outside synovial cavity forming a mass lesion with ill defined margin extending above up to the anterior aspect of lower thigh. Focal hyper intense areas were seen in the condyles of tibia and femur on PDFS and STIR images suggesting bone oedema. Bony irregularities were also noted in the tibial and femoral condyles with joint space narrowing. All menisci and ligaments of the knee joint were of normal configuration and signal intensity. All these findings suggested this to be a case pigmented villonodular synovitis (PVNS) of right knee joint. X ray showed osteoarthritic changes of knee joint.
PVNS is a benign proliferative disorder of uncertain etiology that affects synovial lined joints, bursae, and tendon sheaths. The disorder results in various degrees of villous and/or nodular changes in the affected structures. PVNS lesions are monoarticular or solitary. Polyarticular disease is uncommon but more likely in children. It can be localized or diffuse. The probable causes are inflammation, response to previous trauma, repeated haemorrhages in the affected joint, lipid metabolism disorder and neoplsia.
Radiographs show joint effusion and bone erosions, CT and ultrasound demonstrate hypertrophic synovium as a slightly hyperdense/ echogenic soft tissue mass.
MR images demonstrate mass like synovial proliferation with lobulated margins ranging from low signal through isointense to hyperintense signals on spin-echo images, reflecting the presence of blood and its degradation products. Hemosiderin appears as low signal on T1 and T2 weighted images making it difficult to differentiate calcifications from hemosiderin laden foci; plain films help to confirm or deny the presence of calcifications. A combination of plain films and MRI is used in preoperative evaluation to yield an accurate diagnosis and maps out the extent of disease. MRI findings are characteristic, but not pathognomonic.
The primary treatment options include surgical resection via synovectomy or radiation therapy. Recurrence is reduced with complete resection and often with localized disease. Radiation therapy may be used as the primary treatment method or in concert with surgical resection.


 Subsequently MRI and X-ray of right knee joint was done at Radiology Department. On MRI, right knee joint was found swollen, numerous irregular heterogeneous and mixed signal intensity areas were noted within and outside synovial cavity forming a mass lesion with ill defined margin extending above up to the anterior aspect of lower thigh. Focal hyper intense areas were seen in the condyles of tibia and femur on PDFS and STIR images suggesting bone oedema. Bony irregularities were also noted in the tibial and femoral condyles with joint space narrowing. All menisci and ligaments of the knee joint were of normal configuration and signal intensity. All these findings suggested this to be a case pigmented villonodular synovitis (PVNS) of right knee joint. X ray showed osteoarthritic changes of knee joint.
Subsequently MRI and X-ray of right knee joint was done at Radiology Department. On MRI, right knee joint was found swollen, numerous irregular heterogeneous and mixed signal intensity areas were noted within and outside synovial cavity forming a mass lesion with ill defined margin extending above up to the anterior aspect of lower thigh. Focal hyper intense areas were seen in the condyles of tibia and femur on PDFS and STIR images suggesting bone oedema. Bony irregularities were also noted in the tibial and femoral condyles with joint space narrowing. All menisci and ligaments of the knee joint were of normal configuration and signal intensity. All these findings suggested this to be a case pigmented villonodular synovitis (PVNS) of right knee joint. X ray showed osteoarthritic changes of knee joint.